What is Wrong?
Hip pain can be felt in the groin or in the side or back of the hip. It can radiate down the leg and sometimes it feels “deep” within the joint. Hip pain can come from a variety of pathologies. Some of the most common are:
- Osteoarthritis
- Gluteal Tendinopathy or Greater Trochanteric Bursitis
- Femoroacetabular Impingement or Labral Tears
- Pubalgia
Hip Pain from Osteoarthritis
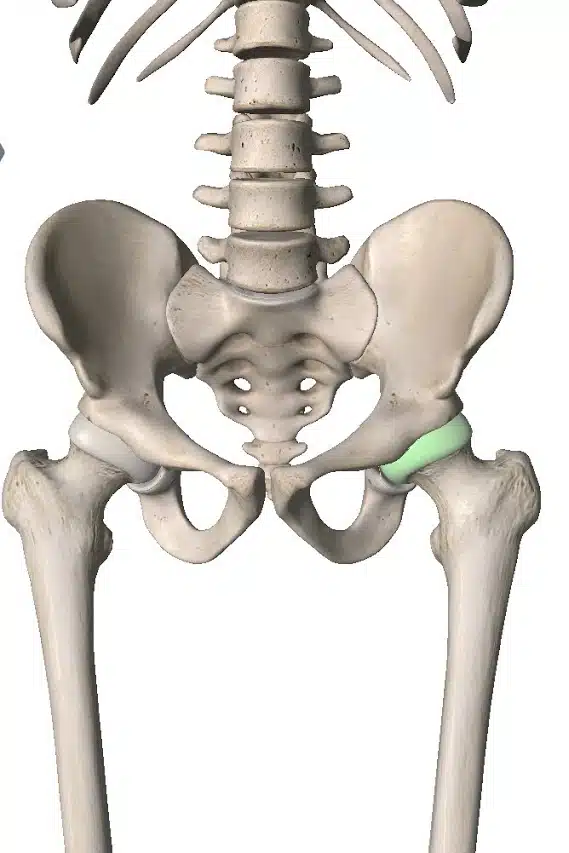
The hip joint is a ball and socket joint. The ball is the head of the femur (thigh bone) and the socket is the acetabulum (part of the pelvis). This joint has a hard smooth lining of articular cartilage that allows the ball to slide around in the socket as we move. Sometimes that lining of cartilage starts to become thinner. This can lead to degeneration of the bone underneath and narrowing of the joint space. Sometimes extra bits of bone grow that are called osteophytes.
Hip Osteoarthritis is a degenerative problem. As it worsens you will experience hip pain and reduced range of movement. The pain is usually felt in the groin but can be anywhere around the hip. It’s usually a problem for older people but can affect younger people if they have had genetic hip problems.
Gluteal Tendinopathy or Greater Trochanteric Bursitis
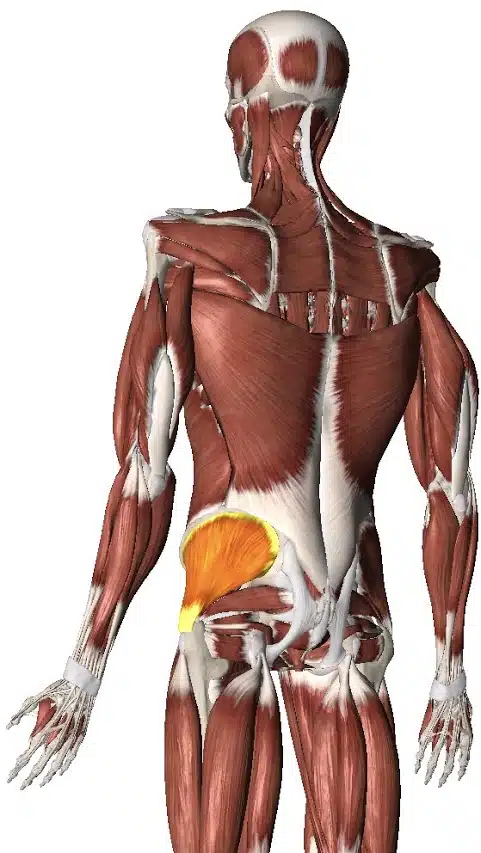
If you put your hand right on the side of your hip that hard sticky-out bone is part of the femur (thigh bone) called the greater trochanter. Some of your gluteal muscles attach to that trochanter. Muscles become tendons before they attach to bones so it’s actually the gluteal tendons that attach to the trochanter. Between the gluteal tendons we have bursae. These are little fluid filled sacks that stop tendons rubbing on other stuff.
Sometimes those tendons can become painful and we call that Gluteal Tendinopathy. Alternatively, the little fluid filled sacks can become inflamed and we call that Greater Trochanteric Bursitis. It can be difficult to tell which is the problem as these pathologies feel similar and often occur together.
Gluteal Tendinopathy and Greater Trochanteric Bursitis usually can pain right on the side of the hip and not elsewhere. These problems are more common in women and more common in the middle-aged population.
Femoroacetabular Impingement or Labral Tears
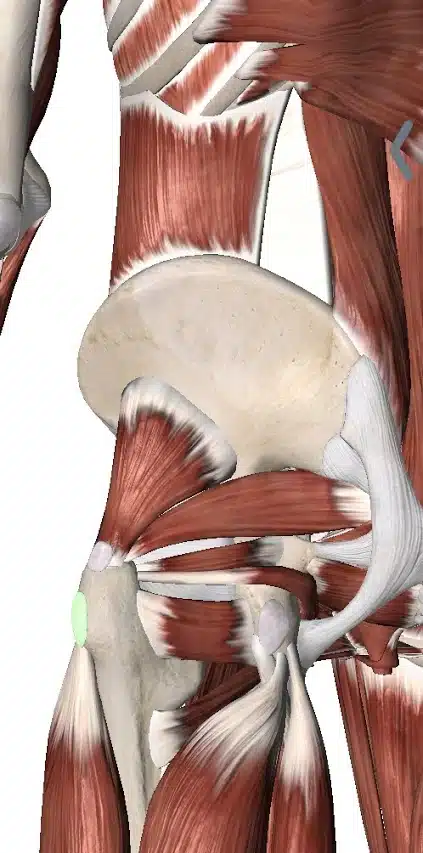
As we’ve discussed the hip joint is between the femur (thigh bone) and the acetabulum (part of the pelvis). We know that articular cartilage lines the joint and makes it smooth. We also have some tissue around the edge of the socket called the Labrum. The labrum deepens the socket and helps keep the head of the femur snuggly nestled inside.
As we lift the knee up towards our chest the hip flexes. This brings the neck of the femur into contact with the acetabulum of the pelvis, squashing the labrum in between. Sometimes, those parts of the pelvis, femur and labrum become irritated and painful. We call that Femoroacetabular Impingement (FAI). Sometimes the labrum becomes torn or frayed. This can cause pain and “clunking” in the hip and we call that a Labral Tear.
Pain from these conditions is almost always felt in the groin area but it can be elsewhere around the hip. This is usually a problem for young people and teenagers. Certain types of bony anatomy of the hip can make it more likely someone will develop these problems (but it doesn’t guarantee it).

Pubalgia
In the groin area the muscles of the inner thigh (adductors) and the muscles of the abdomen attach to the Pubis. This is the front part of the pelvis. The two sides of the pelvis join in the middle via the Pubic Symphysis. There are also various connective tissues in the area such as the Inguinal Ligament.
Damage, tearing or irritation of any of these structures can produce groin pain. There have been lots of terms used to describe these different pathologies over the years (Gilmore’s Groin, Sports Hernia etc.). Pubalgia is more of an umbrella term to describe any of these problems rather than a specific diagnosis.
Pubalgia is usually a problem for the young and sporty population. It is common in teenagers who play hockey, football, soccer and other such sports. It usually manifests as pain in the groin area during or after activity.

How Long Will my Hip Pain Last?
That really depends on what the pathology is. Hip Osteoarthritis can last for years and may slowly get worse over time if not managed properly. Other problems like gluteal tendinopathy or pubalgia may come and go depending on your activities. Unfortunately, not many hip pain problems resolve on their own.
Do I need an x-ray or MRI?
Again, this depends on what pathology is causing your hip pain. Often these conditions can be diagnosed through a clinical examination by a doctor, physiotherapist, chiropractor or athletic therapist. A clinical examination involves physical tests and questions to determine the nature of the problem. This helps narrow the cause down to one of 2-3 potential causes or can even narrow it down to just one clinical diagnosis.
If it is not 100% clear what the pathology is after the clinical examination then you may be referred for imaging. Imaging includes things like x-rays, MRIs, CT or ultrasound scans. These images help the clinician determine what the pathology is.
If an appropriate treatment plan can be made from the clinical examination then there is no need to get imaging studies done. This is usually the case. Since most problems will respond well to conservative management the first port of call is usually rehabilitation. If you are not improving within a reasonable period of time then it may be worth reviewing the clinical diagnosis and the treatment plan. At that point your clinician may refer you for imaging.
It is important to note that clinicians should only refer people for imaging if the results of the imaging would change the treatment plan. For example, your clinician may perform a clinical examination and then say:
“Well, it’s either FAI or pubalgia. Either way I’d recommend 6 weeks of Athletic Therapy”
In this case imaging would not be helpful as the treatment plan would be the same regardless of the results. However, after the clinical exam your clinician could say:
“It looks like gluteal tendinopathy, but I’m a bit worried it might be osteoarthritis. If it’s osteoarthritis I’m going to refer you to a surgeon. If it’s gluteal tendinopathy you can go for Physio. So we’ll order an x-ray to see if it’s osteoarthritis”
In this situation, the results of the imaging would influence the treatment plan. So it is appropriate to order the scan.
What should I do?
There are lots of things you can do to make this less unpleasant and speed up the resolution of your pain. What you ultimately decide to do will depend on your circumstances.
Consult a Professional
This would certainly be my top pick. While the other things on this list will definitely be helpful, there really is no substitute for the guidance and expertise of a professional. It’s like doing your tax return, you can certainly do it yourself, but it would be much easier and more effective to consult an accountant. So the first question is which type of professional? This is where I’m going to show my own bias a little. As a physiotherapist, I honestly feel like a rehabilitation professional such as a Physio, Athletic Therapist or Chiropractor would be the best person to see first.
These professionals can do a full assessment and provide a clinical diagnosis. They can refer you to the appropriate doctors or surgeons for scans and further testing if they feel it is needed. They can also help you understand the problem and design a rehabilitation program that will help you recover as fast as possible.
We have all of these professionals available here at Collegiate Sports Medicine. If you would like to have a chat with us about how we might be able to help, we’d love to hear from you. Just give us a call.
Symptom Guided Activity
This may sound like a strange term. The idea is to stay active but only to the degree that you feel able. I like to use a green light, orange light and red light system. Green is no pain, orange is mild pain and red is severe pain. Generally speaking, you can do whatever you want as long as you feel no pain or mild pain. If the pain becomes severe, you have to stop. Over time, you will find you are able to be more and more active.
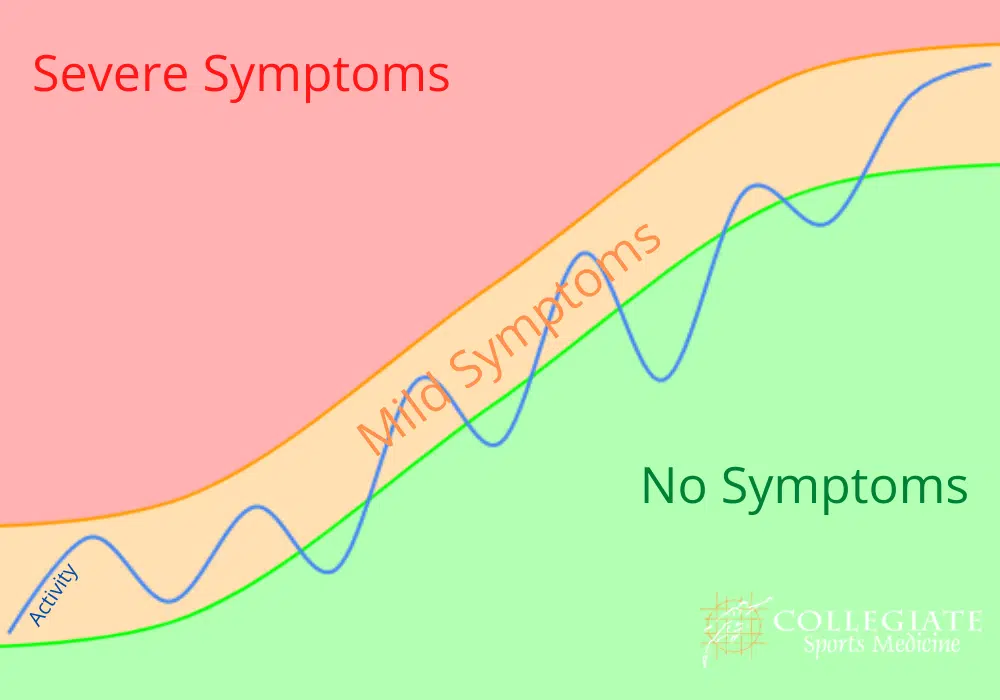
In this sense, no activity is “off limits.” You can go to work, play sports, go for a run, lift weights, go swimming, go camping … whatever you like. Your only restriction is that you must try to avoid that severe “red light” pain. If doing any of these causes severe pain, then leave it till next week and try again!
Manual Therapy
Manual Therapy includes treatments like soft tissue massage and joint mobilisations. There are many different kinds of therapy and different therapists who will have different skills.This is certainly something you may discuss with your therapist should you decide to work with a professional. There are a few things you can do at home such as using a tennis or lacrosse ball to help loosen up the muscles. Again, the traffic light rules apply. There should be no severe “red light” pain. If there is, you need to go more gently.
Just press the ball up against the glutes between you and a wall or the floor. Move around to work the ball as if the ball is giving you a massage. You can do this for as long as you like but I would suggest starting with about 3 minutes and then see how you feel afterwards.
Summary
Hip pain can be coming from a variety of different causes or pathologies. It is not really possible to diagnose it accurately on your own. You would need the input of a doctor, physiotherapist, chiropractor or athletic therapist. The best way to manage the problem really depends on what the diagnosis is. If you would like some advice just give us a call.

