What is causing my foot pain?
Foot pain can come from a variety of pathologies. Some of the most common are:
- Plantar Fasciitis / Fasciopathy
- Achilles Tendonitis / Tendinopathy
- Metatarsalgia
- Morton’s neuroma
- Bunions / Hallux Valgus
Plantar Fasciitis / Fasciopathy
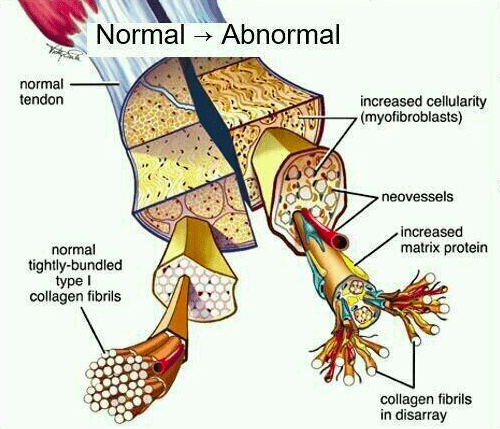
The plantar fascia is a band of connective tissue that supports the arch of the foot. From the calcaneus (heel bone) it fans out and inserts into all the metatarsal heads (toes). The plantar fascia is made of the connective tissue collagen. This is similar to the collagen we have in our ligaments and tendons.
Sometimes the plantar fascia becomes sensitive and painful close to where it attaches to the calcaneus (heel bone). This causes pain in the heel on the underside of the foot.
The pain in the heel is usually worse first thing in the morning. People often limp for the first few steps out of bed. It affects people of all ages but is more common in middle aged people who are physically active or have jobs that involve being on your feet all day.
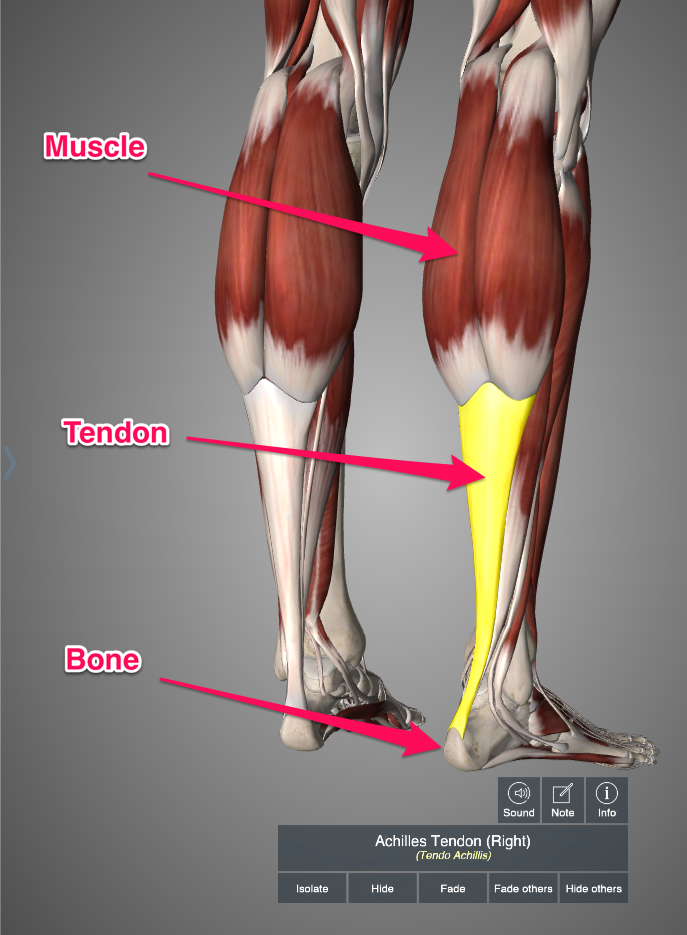
Achilles Tendonitis / Tendinopathy
The calf muscles are called the gastrocnemius and soleus. They come together to form the Achilles Tendon which attaches to the calcaneus (heel bone). Tendons are the stiff, fibrous parts of muscles that attach to bones.
Sometimes that Achilles tendon becomes sensitive and painful. We call this problem Achilles Tendinopathy but it is often referred to as Achilles Tendonitis. Tendinopathy refers to changes in the cellular structure of the tendon. The collagen bundles that make up the tendon become disorganized and sensitive.
Achilles Tendinopathy is more common in middle aged people who are physically active and is very common in runners. The pain is more on the back of the heel (as opposed to underneath the foot). When exercising the pain is usually worse at first but “warms up” and feels better – only to be worse again afterwards.
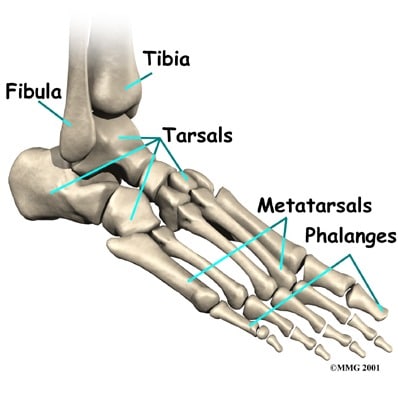
Metatarsalgia
The metatarsal bones of the foot joint the back of the foot to the toes. You have five metatarsal bones in each foot. The metatarsal joins to the phalanx (toe bone) at the metatarsophalangeal joint. Sometimes people call this area the “ball of the foot”.
The ends of those metatarsal bones that connect to the phalanges (toe bones) are called the metatarsal heads. Sometimes the underside (plantar side) of the metatarsal heads becomes irritated and painful. We call that metatarsalgia.
Metatarsalgia manifests as pain in the “ball of the foot” area. It gets worse with lots of time on the feet or running/jumping. It’s rare in young people and more common in the middle and older aged.
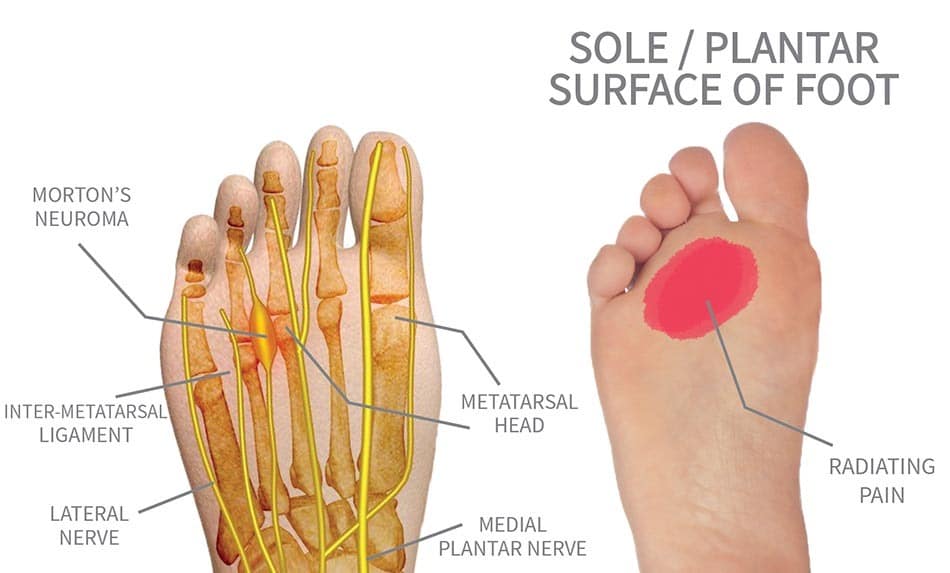
Morton’s Neuroma
In our foot we have little nerves running between the metatarsal bones called the common plantar digital nerves. Sometimes one of those nerves becomes irritated and thickened. This causes pain in the underside of the foot (ball of the foot). It can also cause numbness in the toes.
Morton’s Neuroma typically affects middle-aged people and it’s far more common in women than in men.
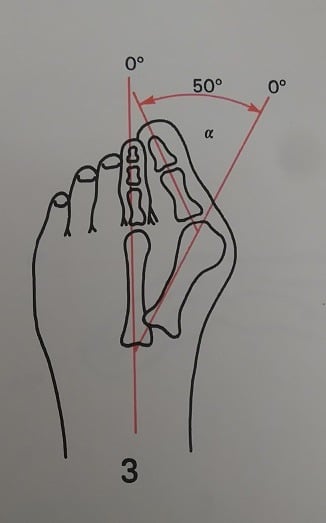
Bunions / Hallux Valgus
The big toe is also called the first digit of the foot. The toe is the phalanx bone and it joins the first metatarsal at the first metatarsophalangeal joint (MTP). An unfortunately common problem is that the joint slowly subluxes (move out of position) over time. Extra tissue known as exostosis develops around the medial (inner) side of the joint. This creates a deformity known as hallux valgus. This problem is commonly referred to as a bunion.
Bunions cause pain within that subluxed MTP joint. They are more common as we age and affect women 10 times more frequently than men.
Do I need an x-ray or MRI?
This depends on what pathology is causing your pain. Often these conditions can be diagnosed through a clinical examination by a doctor, physiotherapist, chiropractor or athletic therapist. A clinical examination involves physical tests and questions to determine the nature of the problem. This helps narrow the cause down to one of 2-3 potential causes or can even narrow it down to just one clinical diagnosis.
If it is not 100% clear what the pathology is after the clinical examination then you may be referred for imaging. Imaging includes things like x-rays, MRIs, CT or ultrasound scans. These images help the clinician determine what the pathology is.
If an appropriate treatment plan can be made from the clinical examination then there is no need to get imaging studies done. This is usually the case. Since most problems will respond well to conservative management the first port of call is usually rehabilitation. If you are not improving within a reasonable period of time then it may be worth reviewing the clinical diagnosis and the treatment plan. At that point your clinician may refer you for imaging.
It is important to note that clinicians should only refer people for imaging if the results of the imaging would change the treatment plan. For example, your clinician may perform a clinical examination and then say:
“Well, it’s either plantar fasciopathy or Achilles tendinopathy. Either way I’d recommend 6 weeks of Athletic Therapy”
In this case imaging would not be helpful as the treatment plan would be the same regardless of the results. However, after the clinical exam your clinician could say:
“It looks like metatarsalgia but I’m a bit worried it might be Morton’s neuroma. If it’s a neuroma I’m going to refer you to a specialist. If it’s metatarsalgia you can go for Physio. So we’ll order an x-ray and an ultrasound to see which it is”
In this situation, the results of the imaging would influence the treatment plan. So it is appropriate to order the scan.
What should I do?
There are lots of things you can do to make this less unpleasant and speed up the resolution of your pain. What you ultimately decide to do will depend on your circumstances.
Consult a Professional
This would certainly be my top pick. While the other things on this list will definitely be helpful, there really is no substitute for the guidance and expertise of a professional. It’s like doing your tax return, you can certainly do it yourself, but it would be much easier and more effective to consult an accountant. So the first question is which type of professional? This is where I’m going to show my own bias a little. As a physiotherapist, I honestly feel like a rehabilitation professional such as a Physio, Athletic Therapist or Chiropractor would be the best person to see first.
These professionals can do a full assessment and provide a clinical diagnosis. They can refer you to the appropriate doctors or surgeons for scans and further testing if they feel it is needed. They can also help you understand the problem and design a rehabilitation program that will help you recover as fast as possible.
We have all of these professionals available here at Collegiate Sports Medicine. If you would like to have a chat with us about how we might be able to help, we’d love to hear from you. Just give us a call.
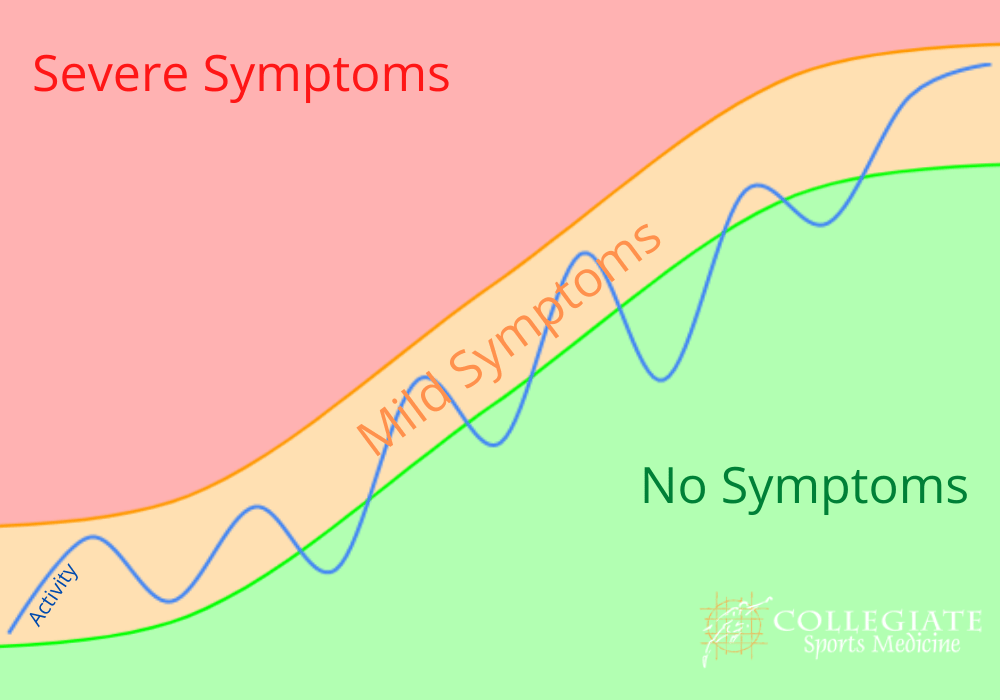
Symptom Guided Activity
This may sound like a strange term. The idea is to stay active but only to the degree that you feel able. I like to use a green light, orange light and red light system. Green is no pain, orange is mild pain and red is severe pain. Generally speaking, you can do whatever you want as long as you feel no pain or mild pain. If the pain becomes severe, you have to stop. Over time, you will find you are able to be more and more active.
In this sense, no activity is “off limits.” You can go to work, play sports, go for a run, lift weights, go swimming, go camping … whatever you like. Your only restriction is that you must try to avoid that severe “red light” pain. If doing any of these causes severe pain, then leave it till next week and try again!
Summary
Elbow pain can be coming from a variety of different causes or pathologies. It is not really possible to diagnose it accurately on your own. You would need the input of a doctor, physiotherapist, chiropractor or athletic therapist. The best way to manage the problem really depends on what the diagnosis is. If you would like some advice just give us a call.